Revolutionizing Health Insurance Claims
Imagine a world where health insurance claims are processed effortlessly, accurately, and in real-time.

Lightning-Fast Processing
Say goodbye to backlogs and delays. Our AI engine analyzes and processes claims in real-time and improving customer satisfaction.

Unmatched Accuracy
Minimize errors and prevent fraudulent claims with our intelligent fraud detection algorithms, ensuring accurate and efficient payouts

Significant Cost Reduction
Automate repetitive tasks, reduce manual labor, and minimize processing costs, freeing up resources for strategic initiatives
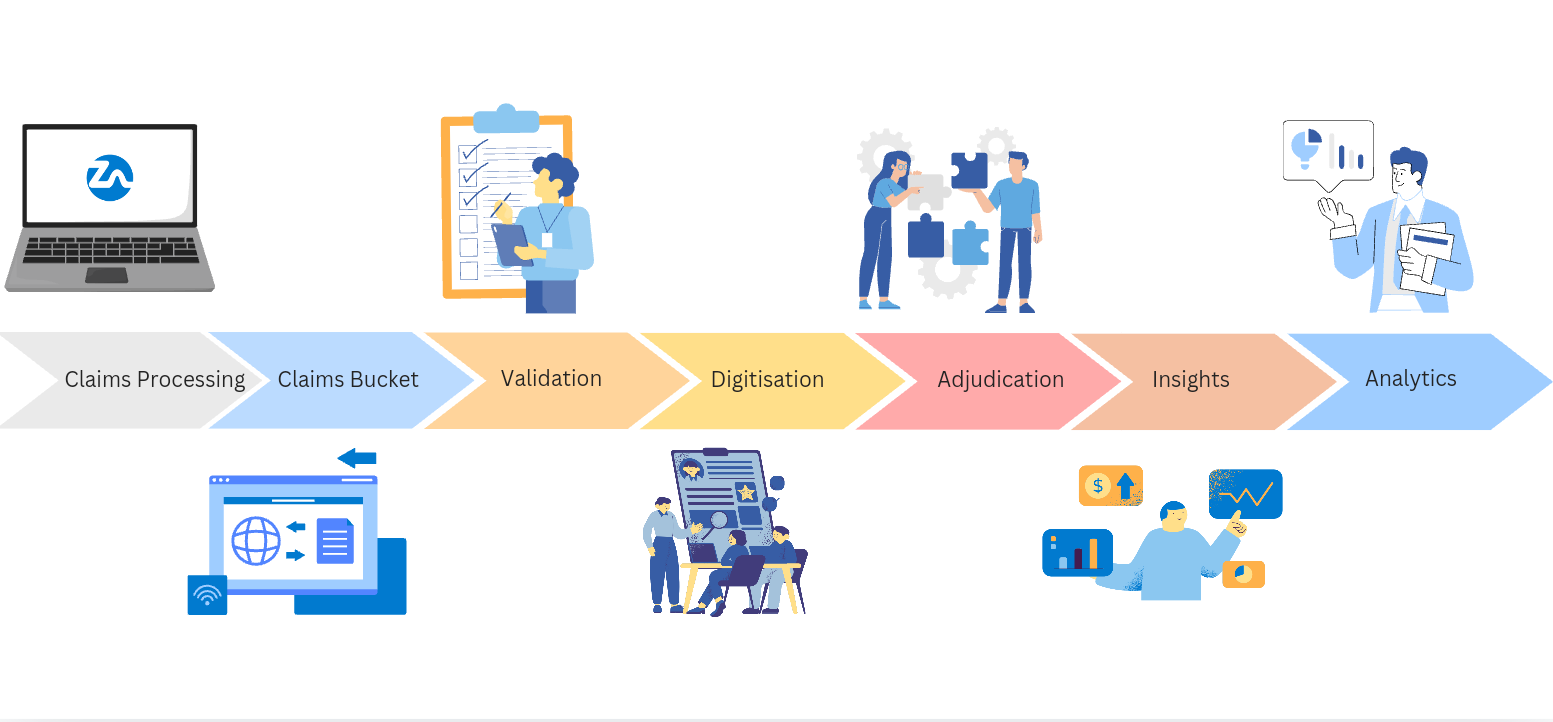
How We’re Changing the Game
Our cutting-edge platform leverages the latest in AI and ML to transform your claims operations

Intelligent Document Processing
Drastically reduce errors and manual data entry, saving time and money. Intelligent processing ensures accurate reimbursements and streamlines workflows. Experience the future of superfast claims with minimal human involvement, maximizing efficiency and minimizing costs. Empower your team to focus on strategic initiatives, not tedious tasks. Unleash the power of intelligent claims processing today.
Error & Fraud Detection
Advanced machine learning algorithms that identify anomalies and suspicious patterns, minimizing errors and preventing fraudulent claims.Uncover hidden manipulations and ensure genuine claims. Advanced techniques detect forgeries, alterations, and inconsistencies in claim documents. Protect your bottom line by identifying fraudulent activities early.


Automated Adjudication
Intelligent algorithms analyze claims against policy guidelines and medical necessity criteria, ensuring accurate and compliant payouts. Leverage precise tariff validation for correct payment calculations, potentially reducing overpayments by up to 10%. This automated approach not only reduces overpayments but also streamlines claims processing, leading to faster turnaround times and improved patient satisfaction.
Tariff Digitisation
Hospital tariff digitisation unlocks a treasure trove of insights for insurance companies. Hospital data analytics empowers insurers to identify cost-saving opportunities, such as directing policyholders to hospitals with lower costs for specific procedures or identifying instances where outpatient care is a viable alternative to hospitalisation. This data-driven approach helps optimise claims processing, potentially reducing processing time by 25-30% and saving insurers millions of dollars annually.


Data-Driven Decisions
Unlock valuable insights into claims trends, key trends and anomalies, identify cost drivers, and optimize your operations for greater efficiency.Access immediate data and analytics at the point of processing, enabling faster, more informed decisions. Real-time analytics to put actionable intelligence directly into the hands of your claims professionals.
Testimonials
See what people have to say about us

Senior Manager
Australian Health Insurance Company
Highly recommended!
There are few that are so focused on the work and ensure the application prove the promise pitched. Zscore have ticked all the boxes. They have a team focused on delivery and are great communicators.

Chief Data Officer
Indian Health Insurance Company
High speed of execution
The Zscore team had worked with us during my tenure at our company where they performed a Proof of Concept on some of the company’s health claims data and gave us some staggering results.

Chief Executive Officer
Indian Health Insurance Company
Customer centric
The Zscore solution was implemented in our organisation successfully with no major setbacks working with all the stakeholders and they handled challenges with patience and diligence.

General Manager
Indian Health Insurance Company
Exceptional Efficiency
We were able to improve our MIS team’s efficiency by about 40%, in certain cases this was 90% or higher. Certain jobs that used to run for 2 hours now run in 2mins, and substantially improved data quality. Our teams now process data directly from Zscore with almost zero manual work..
Our Customers Are Seeing 10X ROI. Here’s How
By streamlining claims processing, reducing errors, and preventing fraud, our customers are experiencing significant cost savings and increased efficiency, resulting in a remarkable 10X return on their investment.
Don’t just imagine the possibilities. Book a demo and experience Zscore in action.

Frequently Asked Questions
Are the Zscore Claims digitisation, adjudication and fraud discovery solutions available individually?
Yes, all our solutions like Digitisation, adjudication, fraud detection, hospital tariff and
Underwriting are available individually and as a complete solution. Enterprises can now pick and choose based on their needs.
Does Zscore provide an API interface to the internal Claims management platforms in enterprises?
Yes, Zscore provides a REST API interface for all the solutions viz. digitisation, adjudication, fraud discovery and underwriting. The processed results are available as a JSON in addition to other formats such as files and as reports & dashboards.
Can the Zscore application be installed under the organisation network to ensure data security?
The Zscore application can be easily installed on a private cloud within the organisation. Zscore takes the customer data privacy seriously and encourages organisations to have the product installed in its own IT network.
What are the customisations that needs to be done during installation?
Zscore requires zero customisation. All Zscore solutions are ready to go live. Most
customisations generally happen during API integration or when custom requirements are provided to suit local customer needs.
Revolutionizing Health Insurance Claims
Book a demo call today to witness the future of data-driven innovation


